Abstract
Purpose
We evaluated the changes in the strain energy density (SED) in the temporomandibular joint (TMJ) disk after sagittal split ramus osteotomy (SSRO) at three time points. A finite element model (FEM) based on real patient-based computed tomography (CT) data was used to examine the effect of SSRO on the TMJ.
Methods
Measurements of the condylar position and angulation in CT images and FEM analyses were performed for 17 patients scheduled to undergo SSROs at the following time points: before surgery, immediately after surgery, and 1 year after surgery. SED on the entire disk was calculated at each of the three time points using FEM. Furthermore, the relationship between individual SED values and the corresponding condylar position was also evaluated.
Results
No significant change was observed in the condylar position at the three time points. The FEM analysis showed that SED was the highest and lowest immediately after and 1 year after surgery, respectively. A possible SED distribution imbalance between the left and right joints was improved 1 year after SSRO. Concerning the effect of fossa morphometry and condylar position, wide and deep glenoid fossae and a more posterior condylar position tended to show lower SED.
Conclusion
SED in the articular disk temporarily increased after surgery and significantly decreased 1 year after surgery compared with that before surgery. SSRO generally improved the imbalance between the left and right joints. Thus, SSRO, which improves maxillofacial morphology, may also improve components of temporomandibular disorders.
Zusammenfassung
Zielsetzung
Wir untersuchten die Veränderungen der Dehnungsenergiedichte (SED) im Discus articularis des Temporomandibulargelenks (TMJ) nach einer sagittalen Ramus-Split-Osteotomie (SSRO) zu 3 Zeitpunkten. Ein Finite-Elemente-Modell (FEM), das auf realen, patientenbasierten Computertomographiedaten (CT) basiert, wurde verwendet, um die Auswirkungen der SSRO auf das TMJ zu ermitteln.
Methoden
Bei 17 Patienten, bei denen eine SSRO geplant war, wurden Messungen der Kondylenposition und -angulation auf CT-Bildern und FEM-Analysen zu den folgenden Zeitpunkten durchgeführt: präoperativ, direkt nach der Operation und ein Jahr postoperativ. Die SED des gesamten Discus articularis wurde für jeden der 3 Untersuchungszeitpunkte mittels FEM berechnet. Darüber hinaus wurde auch die Beziehung zwischen den einzelnen SED-Werten und der entsprechenden Kondylenposition bewertet.
Ergebnisse
Zu den 3 Zeitpunkten wurde keine signifikante Veränderung der Kondylenposition beobachtet. Die FEM-Analyse zeigte, dass die SED unmittelbar postoperativ und ein Jahr nach der Operation am höchsten bzw. am niedrigsten war. Ein mögliches Ungleichgewicht der SED-Verteilung zwischen linkem und rechtem Gelenk war ein Jahr nach der SSRO verbessert. Was den Einfluss der Fossamorphometrie und der Kondylenposition betrifft, so zeigte sich bei breiter und tiefer Fossa glenoidalis und einer eher posterioren Kondylenposition tendenziell eine niedrigere SED.
Schlussfolgerung
Die SED in der Gelenkscheibe nahm nach der Operation vorübergehend zu und ging ein Jahr nach der Operation im Vergleich zur Zeit vor der Operation deutlich zurück. Die SSRO verbesserte generell das Ungleichgewicht zwischen dem linken und dem rechten Gelenk. Somit kann die SSRO, welche die maxillofaziale Morphologie verbessert, auch an temporomandibulären Störungen beteiligte Faktoren verbessern.





Similar content being viewed by others
References
Pruitt JW, Moenning JE, Lapp TH, Bussard DA (2002) Treatment of painful temporomandibular joint dysfunction with the sagittal split ramus osteotomy. J Oral Maxillofac Surg 60:996–1102. https://doi.org/10.1053/joms.2002.34405
Nishimura M, Segami N, Sato J, Honjou M, Fujimura K (2004) Transitional joint effusion in the mandibular prognathic surgery patient: intraoral vertical ramus osteotomy versus sagittal split ramus osteotomy. J Oral Maxillofac Surg 62:545–548. https://doi.org/10.1016/j.joms.2003.06.015
Zhao Q, Hu J, Wang D, Zhu S (2007) Changes in the temporomandibular joint after mandibular setback surgery in monkeys: Intraoral vertical versus sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104:329–337. https://doi.org/10.1016/j.tripleo.2006.12.024
Westermark A, Shayeghi F, Thor A (2001) Temporomandibular dysfunction in 1,516 patients before and after orthognathic surgery. Int J Adult Orthodon Orthognath Surg 16:145–151
Pahkala R, Heino J (2004) Effect of sagittal split ramus osteotomy on temporomandibular disorders in seventy-two patients. Acta Odontol Scand 62:238–244. https://doi.org/10.1080/00016350410001667
Aoyama S, Kino K, Kobayashi J, Yoshimura H, Amagasa T (2005) Clinical evaluation of the temporomandibular joint following orthognathic surgery—multiple logistic regression analysis. J Med Dent Sci 52:109–111
Kim YK, Yun PY, Ahn JY, Kim JW, Kim SG (2009) Changes in the temporomandibular joint disc position after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:15–21. https://doi.org/10.1016/j.tripleo.2009.02.005
Dervis E, Tuncer E (2002) Long-term evaluations of temporomandibular disorders in patients undergoing orthognathic surgery compared with a control group. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:554–560. https://doi.org/10.1067/moe.2002.128021
Fang B, Shen GF, Yang C, Wu Y, Feng YM, Mao LX, Xia YH (2009) Changes in condylar and joint disc positions after bilateral sagittal split ramus osteotomy for correction of mandibular prognathism. Int J Oral Maxillofac Surg 38:726–730. https://doi.org/10.1016/j.ijom.2009.03.001
Okeson JP (2013) Management of temporomandibular disorders and occlusion, 7th edn. Mosby, St. Louis, MO
Ueki K, Nakagawa K, Takatsuka S, Yamamoto E (2006) The change of stress distribution on the condyle after mandibular setback surgery. Eur J Orthod 28:433–439. https://doi.org/10.1093/ejo/cjl003
Ueki K, Marukawa K, Moroi A, Sotobori M, Ishihara Y, Iguchi R, Kosaka A, Nakano Y, Higuchi M, Nakazawa R et al (2014) Evaluation of overlapped cortical bone area after modified plate fixation with bent plate in sagittal split ramus osteotomy. J Craniomaxillofac Surg 42:e210–e216. https://doi.org/10.1016/j.jcms.2013.08.009
Zhao C, Kurita H, Kurashina K, Hosoya A, Arai Y, Nakamura H (2010) Temporomandibular joint response to mandibular deviation in rabbits detected by 3D micro-CT imaging. Arch Oral Biol 55:929–937. https://doi.org/10.1016/j.archoralbio.2010.07.019
Panula K, Somppi M, Finne K, Oikarinen K (2000) Effects of orthognathic surgery on temporomandibular joint dysfunction: a controlled prospective 4‑year follow-up study. Int J Oral Maxillofac Surg 29:183–187. https://doi.org/10.1016/S0901-5027(00)80089-2
Shu JH, Yao J, Zhang YL, Chong DYR, Liu Z (2018) The influence of bilateral sagittal split ramus osteotomy on the stress distributions in the temporomandibular joints of the patients with facial asymmetry under symmetric occlusions. Medicine 97:e11204. https://doi.org/10.1097/MD.0000000000011204
Liu Z, Shu J, Zhang Y, Fan Y (2018) The biomechanical effects of sagittal split ramus osteotomy on temporomandibular joint. Comput Methods Biomech Biomed Engin 21:617–624. https://doi.org/10.1080/10255842.2018.1504034
Ma H, Shu J, Wang Q, Teng H, Liu Z (2020) Effect of sagittal split ramus osteotomy on stress distribution of temporomandibular joints in patients with mandibular prognathism under symmetric occlusions. Comput Methods Biomech Biomed Engin 23:1297–1305. https://doi.org/10.1080/10255842.2020.1796984
Nickel J, Spilker R, Iwasaki L, Gonzalez Y, McCall WD, Ohrbach R, Beatty MW, Marx D (2009) Static and dynamic mechanics of the temporomandibular joint: plowing forces, joint load and tissue stress. Orthod Craniofac Res 12:159–167. https://doi.org/10.1111/j.1601-6343.2009.01449.x
Colombo V, Palla S, Gallo LM (2008) Temporomandibular joint loading patterns related to joint morphology: a theoretical study. Cells Tissues Organs 187:295–306. https://doi.org/10.1159/000113408
Stratmann U, Schaarschmidt K, Santamaria P (1996) Morphometric investigation of condylar cartilage and disc thickness in the human temporomandibular joint: significance for the definition of osteoarthritic changes. J Oral Pathol Med 25:200–205. https://doi.org/10.1111/j.1600-0714.1996.tb01372.x
Oberg T, Carlsson GE, Fajers CM (1971) The temporomandibular joint: a morphologic study on human autopsy material. Acta Odontol Scand 29:349–384. https://doi.org/10.3109/00016357109026526
Gallo LM, Iwasaki LR, Gonzalez YM, Liu H, Marx DB, Nickel JC (2015) Diagnostic group differences in temporomandibular joint energy densities. Orthod Craniofac Res 18:164–169. https://doi.org/10.1111/ocr.12074
Wagner A, Krach W, Schicho K, Undt G, Ploder O, Ewers R (2002) A 3‑dimensional finite-element analysis investigating the biomechanical behavior of the mandible and plate osteosynthesis in cases of fractures of condylar process. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:678–686. https://doi.org/10.1067/moe.2002.126451
Lovald S, Baack B, Gaball C, Olson G, Hoard A (2010) Biomechanical optimization of bone plates used in rigid fixation of mandibular symphysis fractures. J Oral Maxillofac Surg 68:1833–1841. https://doi.org/10.1016/j.joms.2009.09.108
Xiangdong Q, Limin MA, Shizhen Z (2012) The influence of the closing and opening muscle groups of jaw condyle biomechanics after mandible bilateral sagittal split ramus osteotomy. J Craniomaxillofac Surg 40:e159–e164. https://doi.org/10.1016/j.jcms.2011.07.024
Murakami K, Yamamoto K, Sugiura T, Kawakami M, Kang YB, Tsutsumi S et al (2013) Effect of clenching on biomechanical response of human mandible and temporomandibular joint to traumatic force analyzed by finite element method. Med Oral Patol Oral Cir Bucal 18:e473–e478. https://doi.org/10.4317/medoral.18488
Murakami K, Yamamoto K, Sugiura T, Kawakami M, Horita S, Kirita T (2015) Biomechanical analysis of poly-L-lactic acid and titanium plates fixated for mandibular symphyseal fracture with a conservatively treated unilateral condylar fracture using the three-dimensional finite element method. Dent Traumatol 31:396–402. https://doi.org/10.1111/edt.12179
Murakami K, Yamamoto K, Tsuyuki M, Sugiura T, Tsutsumi S, Kirita T (2014) Theoretical efficacy of preventive measures for pathologic fracture after surgical removal of mandibular lesion based on 3‑dimensional finite element analysis. J Oral Maxillofac Surg 72:833.e1–e18. https://doi.org/10.1016/j.joms.2013.12.019
Huiskes R, Weinans H, Grootenboer HJ, Dalstra M, Fudala B, Slooff TJ et al (1987) Adaptive bone-remodeling theory applied to prosthetic-design analysis. J Biomech 20:1135–1150. https://doi.org/10.1016/0021-9290(87)90030-3
Liefeith K, Kaufhold S, Rost J (1998) Untersuchungen zum Einfluss einer prothetischen Versorgung auf die Strain-Energy-Density-Verteilung im Femur. Biomed Tech (Berl) 43:179–183. https://doi.org/10.1515/bmte.1998.43.6.179
Inglam S, Suebnukarn S, Tharanon W, Apatananon T, Sitthiseripratip K (2010) Influence of graft quality and marginal bone loss on implants placed in maxillary grafted sinus: a finite element study. Med Biol Eng Comput 48:681–689. https://doi.org/10.1007/s11517-010-0584-3
Suárez DR, Weinans H, van Keulen F (2012) Bone remodelling around a cementless glenoid component. Biomech Model Mechanobiol 11:903–913. https://doi.org/10.1007/s10237-011-0360-9
Eser A, Tonuk E, Akca K, Cehreli MC (2009) Numeric simulation of time-dependent remodeling of bone around loaded oral implants. Int J Oral Maxillofac Implants 24:597–608
Kumaresan S, Yoganandan N, Pintar FA, Maiman DJ, Goel VK (2001) Contribution of disc degeneration to osteophyte formation in the cervical spine: a biomechanical investigation. J Orthop Res 19:977–984. https://doi.org/10.1016/S0736-0266(01)00010-9
Rosenberg N, Bull AMJ (2018) Simulating localised cellular inflammation and substrate properties in a strain energy density based bone remodelling algorithm for use in modelling trauma. Comput Methods Biomech Biomed Engin 21:208–218. https://doi.org/10.1080/10255842.2018.1439025
Weinans H, Huiskes R, Grootenboer HJ (1992) The behavior of adaptive bone-remodeling simulation models. J Biomech 25:1425–1441. https://doi.org/10.1016/0021-9290(92)90056-7
Ueki K, Marukawa K, Nakagawa K, Yamamoto E (2002) Condylar and temporomandibular joint disk positions after mandibular osteotomy for prognathism. J Oral Maxillofac Surg 60:1424–1432. https://doi.org/10.1053/joms.2002.36098
Lee W, Park JU (2002) Three-dimensional evaluation of positional change of the condyle after mandibular setback by means of bilateral sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:305–309. https://doi.org/10.1067/moe.2002.126452
del Palomar AP, Doblaré M (2006) 3D finite element simulation of the opening movement of the mandible in healthy and pathologic situations. J Biomech Eng 128:242–249. https://doi.org/10.1115/1.2165697
Katona TR (2001) A mathematical analysis of the role of friction in occlusal trauma. J Prosthet Dent 86:636–643. https://doi.org/10.1067/mpr.2001.120068
Korioth TWP, Hannam AG (1994) Mandibular force during simulated tooth clenching. J Orofac Pain 8:178–189
Murakami K, Sugiura T, Yamamoto K, Kawakami M, Kang YB, Tsutsumi S et al (2011) Biomechanical analysis of the strength of the mandible after marginal resection. J Oral Maxillofac Surg 69(6):1798–1806. https://doi.org/10.1016/j.joms.2010.07.052
Keyak JH, Rossi SA, Jones KA, Skinner HB (1998) Prediction of femoral fracture load using automated finite element modeling. J Biomech 31:125–133. https://doi.org/10.1016/S0021-9290(97)00123-1
Kang MG, Yun KI, Kim CH, Park JU (2010) Postoperative condylar position by sagittal split ramus osteotomy with and without bone graft. J Oral Maxillofac Surg 68:2058–2064. https://doi.org/10.1016/j.joms.2009.12.015
Kawamata A, Fujishita M, Nagahara K, Kanematu N, Niwa K, Langlais RP (1998) Three-dimensional computed tomography evaluation of postsurgical condylar displacement after mandibular osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85:371–376. https://doi.org/10.1016/S1079-2104(98)90059-2
Barrientos E, Pelayo F, Tanaka E, Lamela-Rey MJ, Fernández-Canteli A (2016) Dynamic and stress relaxation properties of the whole porcine temporomandibular joint disc under compression. J Mech Behav Biomed Mater 57:109–111. https://doi.org/10.1016/j.jmbbm.2015.12.003
Nickel JC, Iwasaki LR, Gonzalez YM, Gallo LM, Yao H (2018) Mechanobehavior and ontogenesis of the temporomandibular joint. J Dent Res 97:1185–1192. https://doi.org/10.1177/0022034518786469
Koolstra JH, van Eijden TM (2005) Combined finite-element and rigid-body analysis of human jaw joint dynamics. J Biomech 38:2431–2439. https://doi.org/10.1016/j.jbiomech.2004.10.014
Beek M, Koolstra JH, van Ruijven LJ, van Eijden TM (2001) Three-dimensional finite element analysis of the cartilaginous structures in the human temporomandibular joint. J Dent Res 80(10):1913–1918. https://doi.org/10.1177/00220345010800101001
Beek M, Koolstra JH, van Ruijven LJ, van Eijden TM (2000) Three-dimensional finite element analysis of the human temporomandibular joint disc. J Biomech 33:307–316. https://doi.org/10.1016/S0021-9290(99)00168-2
Tanaka E, Hirose M, Inubushi T, Koolstra JH, van Eijden TM, Suekawa Y, Fujita R, Tanaka M, Tanne K (2007) Effect of hyperactivity of the lateral pterygoid muscle on the temporomandibular joint disk. J Biomech Eng 129:890–897. https://doi.org/10.1115/1.2800825
Ellis E, Throckmorton GS (2001) Bite forces after open or closed treatment of mandibular condylar process fractures. J Oral Maxillofac Surg 59:389–395. https://doi.org/10.1053/joms.2001.21873
Karabouta I, Martis C (1985) The TMJ dysfunction syndrome before and after sagittal split osteotomy of the rami. J Maxillofac Surg 13:185–185. https://doi.org/10.1016/S0301-0503(85)80045-X
Upton LG, Scott RF, Hayward JR (1984) Major maxillomandibular malrelations and temporomandibular joint pain-dysfunction. J Prosthet Dent 51:686–690. https://doi.org/10.1016/0022-3913(84)90418-9
Choy SEM, Lenz J, Schweizerhof K, Schmitter M, Schindler HJ (2017) Realistic kinetic loading of the jaw system during single chewing cycles: a finite element study. J Oral Rehabil 44:375–384. https://doi.org/10.1111/joor.12501
Mladenović I, Dodić S, Stošić S, Petrović D, Cutović T, Kozomara R (2014) TMD in class III patients referred for orthognathic surgery: psychological and dentition-related aspects. J Craniomaxillofac Surg 42:1604–1609. https://doi.org/10.1016/j.jcms.2014.04.029
Author information
Authors and Affiliations
Contributions
Kazuhiro Murakami contributed to conception, design, data acquisition, and interpretation; performed all statistical analyses; and drafted and critically revised the manuscript. Kazuhiko Yamamoto contributed to conception and drafted and critically revised the manuscript. Masayoshi Kawakami contributed to conception and design and critically revised the manuscript. Horita Satoshi contributed to conception and drafted and critically revised the manuscript. Kirita Tadaaki contributed to conception and drafted and critically revised the manuscript. All authors gave their final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
K. Murakami, K. Yamamoto, M. Kawakami, S. Horita and T. Kirita declare that they have no competing interests.
Ethical standards
This study was performed in accordance with the principles outlined in the Declaration of Helsinki and was approved by the ethical committee of Nara Medical University (permission number: 410). All patients were informed of the purpose of the study and signed a consent form before inclusion. Furthermore, this study conformed to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
1.
Keyak’s formula
Young’s modulus (MPa) density range (g/cm3)
SED was calculated using the following equations:
(From the formula, SED is determined by the magnitude of stress.)
Substituting the components in each direction,
In the display of strain components only,
(\(U_{0}\) strain energy density; \(\upsigma\) stress; E elastic modulus; \(\upvarepsilon\) normal strain; \(\upgamma\) shear strain; \(\nu\) Poissonʼs ratio)
2.
-
1.
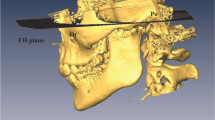
Facial angle (angle between the Frankfort plane and the sella–pogonion)
-
2.
Occlusal plane angle (angle between the Frankfort plane and the occlusal plane)
-
3.
Y‑axis (angle between the Frankfort plane and the sella–gnathion)
-
4.
Convexity (pogonion–nasion–A point angle)
-
5.
Mandibular plane angle (angle between the Frankfort plane and the menton–gonion)
-
6.
Gonial angle, SNA angle (menton–gonion–articulare point angle)
-
7.
SNA angle (sella–nasion–A point angle)
-
8.
SNB angle (sella–nasion–B point angle)
-
9.
ANB angle (A point angle–nasion–B point angle)
3.
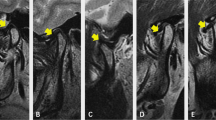
To examine the anteroposterior positional relationship of the condyle in the glenoid fossa, x/X (anteroposterior ratio of the condylar position in the X‑axis) was calculated in our previous study.
The x/X ratio in class 3 (n = 30) was 0.573 and that in class 1 (n = 17) was 0.523. There was a significant difference between the two groups.
4.
Comparison of SED magnitude between patients with and without symptoms in our previous study
Fifty-seven finite element models similar to those in the present study, based on the CT images of each patient, were constructed, and the mean SED in the TMJ disk was calculated. We compared the mean SED between the models with and without TMD symptoms. The magnitude of SED with symptoms (n = 10) was 0.178 MPa and that without symptoms (n = 47) was 0.078 MPa. Significant differences were observed between patients with and without symptoms (p < 0.05; Mann–Whitney U test).
Rights and permissions
About this article
Cite this article
Murakami, K., Yamamoto, K., Kawakami, M. et al. Changes in strain energy density in the temporomandibular joint disk after sagittal split ramus osteotomy using a computed tomography-based finite element model. J Orofac Orthop (2023). https://doi.org/10.1007/s00056-022-00441-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00056-022-00441-3
Keywords
- Finite element analysis
- Temporomandibular joint dysfunction
- Orthognathic surgery
- X‑ray computed tomography
- Cephalometric analysis