Abstract
Purpose
Rapidly destructive coxarthrosis (RDC) is a rare syndrome of unknown etiology. This study evaluated sagittal spinopelvic alignment (SSPA) in patients with RDC and compared it with that in patients with hip osteoarthritis (HOA). In addition, finite element analysis (FEA) was performed to investigate the distribution of stress on the femoral head in RDC versus HOA.
Methods
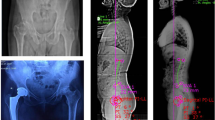
This retrospective study included patients who had undergone primary total hip arthroplasty for RDC (n = 33) and HOA (n = 99; age- and sex-matched to patients with RDC) at three hospitals from June 2014 to September 2020. Preoperative SSPA parameters and inflammatory blood markers were compared between the two groups. FEA on the computed tomography data was performed for four patients from each group with similar pelvic tilt (PT) and lateral center–edge angle (LCEA). The distribution of Drucker–Prager equivalent stress was assessed at the loaded area of the femoral head.
Results
Patients with RDC had significantly higher PT, lower sacral slope, decreased lumbar lordosis (LL), higher sagittal vertical axis, and higher pelvic incidence minus LL than patients with HOA, indicating sagittal spinal imbalance. Blood test revealed patients with RDC had higher levels of inflammation markers than patients with HOA. FEA revealed no statistically significant difference in the degree of stress concentration or the maximum equivalent stress between the two groups when PT and LCEA were comparable.
Conclusion
Patients with RDC tend to have sagittally imbalanced spine. Decreased acetabular coverage of the femoral head may heighten mechanical load of the hip joint in patients with RDC.





Similar content being viewed by others
Data availability
The datasets analyzed in this study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Postel M, Kerboull M (1970) Total prosthetic replacement in rapidly destructive arthrosis of the hip joint. Clin Orthop Relat Res 72:138–144
Mavrogenis AF, Flevas DA, Panagopoulos GN, Megaloikonomos P, Igoumenou V, Vottis C, Sakellariou V, Kontogeorgakos V (2015) Rapid destructive arthritis of the hip revisited. Eur J Orthop Surg Traumatol 25(7):1115–1120. https://doi.org/10.1007/s00590-015-1676-4
Forestier F (1957) Coxite rhumatismales subaigues et chroniques. Thesis
Ogawa K, Mawatari M, Komine M, Shigematsu M, Kitajima M, Kukita A, Hotokebuchi T (2007) Mature and activated osteoclasts exist in the synovium of rapidly destructive coxarthrosis. J Bone Miner Metab 25(6):354–360. https://doi.org/10.1007/s00774-007-0761-0
Menkes CJ, Simon F, Delrieu F, Forest M, Delbarre F (1976) Destructive arthropathy in chondrocalcinosis articularis. Arthritis Rheum 19(Suppl 3):329–348. https://doi.org/10.1002/1529-0131(197605/06)19:3+%3c329::aid-art1780190706%3e3.0.co;2-z
Yamamoto T, Bullough PG (2000) The role of subchondral insufficiency fracture in rapid destruction of the hip joint: a preliminary report. Arthritis Rheum 43(11):2423–2427. https://doi.org/10.1002/1529-0131(200011)43:11%3c2423::Aid-anr8%3e3.0.Co;2-z
Offierski CM, MacNab I (1983) Hip-spine syndrome. Spine (Phila Pa 1976) 8(3):316–321. https://doi.org/10.1097/00007632-198304000-00014
Watanabe W, Sato K, Itoi E, Yang K, Watanabe H (2002) Posterior pelvic tilt in patients with decreased lumbar lordosis decreases acetabular femoral head covering. Orthopedics 25(3):321–324. https://doi.org/10.3928/0147-7447-20020301-16
Morimoto T, Kitajima M, Tsukamoto M, Yoshihara T, Sonohata M, Mawatari M (2018) Sagittal spino-pelvic alignment in rapidly destructive coxarthrosis. Eur Spine J 27(2):475–481. https://doi.org/10.1007/s00586-017-5282-5
Yasuda T, Matsunaga K, Hashimura T, Tsukamoto Y, Sueyoshi T, Ota S, Fujita S, Onishi E (2020) Characterization of rapidly progressive osteoarthritis of the hip in its early stage. Eur J Rheumatol 7(3):130–134. https://doi.org/10.5152/eurjrheum.2020.19159
Onishi E, Ota S, Fujita S, Tsukamoto Y, Yamashita S, Hashimura T, Matsunaga K, Yasuda T (2022) Association between sagittal spinopelvic alignment and femoral head destruction in the early stage of rapidly destructive coxopathy. Bone Jt Open 3(1):77–84. https://doi.org/10.1302/2633-1462.31.Bjo-2021-0175.R1
Kitamura K, Fujii M, Utsunomiya T, Iwamoto M, Ikemura S, Hamai S, Motomura G, Todo M, Nakashima Y (2020) Effect of sagittal pelvic tilt on joint stress distribution in hip dysplasia: a finite element analysis. Clin Biomech (Bristol, Avon) 74:34–41. https://doi.org/10.1016/j.clinbiomech.2020.02.011
Loppini M, Pisano A, Ruggeri R, Della Rocca A, Grappiolo G (2022) Pelvic tilt and functional acetabular position after total hip arthroplasty: an EOS 2D/3D radiographic study. Hip Int. https://doi.org/10.1177/11207000211073668
Okuzu Y, Miyahara T, Goto K, Kuroda Y, Kawai T, Matsuda S (2022) Investigating sagittal spinal alignment, low back pain, and clinical outcomes after total hip arthroplasty for lumbar hyperlordosis: a retrospective study. Arch Orthop Trauma Surg 142(12):4007–4013. https://doi.org/10.1007/s00402-021-04266-4
Utsunomiya T, Motomura G, Ikemura S, Kubo Y, Sonoda K, Hatanaka H, Baba S, Kawano K, Yamamoto T, Nakashima Y (2018) Effects of sclerotic changes on stress concentration in early-stage osteonecrosis: a patient-specific, 3D finite element analysis. J Orthop Res 36(12):3169–3177. https://doi.org/10.1002/jor.24124
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Jt Surg Am 93(11):1057–1063. https://doi.org/10.2106/jbjs.J.00160
Keyak JH, Rossi SA, Jones KA, Skinner HB (1998) Prediction of femoral fracture load using automated finite element modeling. J Biomech 31(2):125–133. https://doi.org/10.1016/s0021-9290(97)00123-1
Hwang D-H, Zum Gahr K-H (2003) Transition from static to kinetic friction of unlubricated or oil lubricated steel/steel, steel/ceramic and ceramic/ceramic pairs. Wear 255(1–6):365–375
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37(12):1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T, Yanagibashi Y (2005) Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 30(14):1650–1657. https://doi.org/10.1097/01.brs.0000169446.69758.fa
Homma Y, Baba T, Sumiyoshi N, Ochi H, Kobayashi H, Matsumoto M, Yuasa T, Kaneko K (2014) Rapid hip osteoarthritis development in a patient with anterior acetabular cyst with sagittal alignment change. Case Rep Orthop 2014:523426. https://doi.org/10.1155/2014/523426
Baba T, Homma Y, Ochi H, Ozaki Y, Matsumoto M, Shitoto K, Kaneko K (2016) Total hip arthroplasty using a Kerboull-type plate for rapidly destructive coxarthrosis: comparison with uncemented acetabular component. Eur J Orthop Surg Traumatol 26(2):189–194. https://doi.org/10.1007/s00590-015-1738-7
Masuhara K, Nakai T, Yamaguchi K, Yamasaki S, Sasaguri Y (2002) Significant increases in serum and plasma concentrations of matrix metalloproteinases 3 and 9 in patients with rapidly destructive osteoarthritis of the hip. Arthritis Rheum 46(10):2625–2631. https://doi.org/10.1002/art.10547
Abe H, Sakai T, Ogawa T, Takao M, Nishii T, Nakamura N, Sugano N (2017) Characteristics of bone turnover markers in rapidly destructive coxopathy. J Bone Miner Metab 35(4):412–418. https://doi.org/10.1007/s00774-016-0769-4
Yasuda T, Matsunaga K, Hashimura T, Tsukamoto Y, Sueyoshi T, Ota S, Fujita S, Onishi E (2020) Bone turnover markers in the early stage of rapidly progressive osteoarthritis of the hip. Eur J Rheumatol 8(2):57–61. https://doi.org/10.5152/eurjrheum.2020.20046
Acknowledgements
The authors would like to thank Hideyuki Mimata, Research Center of Computational Mechanics, Inc. for their technical advice on FEM analysis.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
KO and YO collected and interpreted the patient data. KO were major contributors in writing the manuscript. TS, TK, YK, KG, and SM were involved in report design, critically revised the report, and commented on drafts of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Shuichi Matsuda has received speaker and consultant honoraria from Kyocera. Other authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Kyoto University approved this study.
Consent to participate
Informed consent was waived in this study.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Orita, K., Okuzu, Y., Shimizu, T. et al. Investigating sagittal spinopelvic alignment and equivalent stress on the femoral head in patients with rapidly destructive coxarthrosis. Eur J Orthop Surg Traumatol 34, 901–908 (2024). https://doi.org/10.1007/s00590-023-03733-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03733-5